Did you know almost 1.6 million Americans have Type 1 Diabetes, often called juvenile diabetes? This illness happens when the body’s immune system wrongfully attacks insulin-making beta cells in the pancreas. This leads to the production of little or no insulin.
Insulin is vital because it helps glucose enter cells to create energy. Without it, blood sugar levels can get too high, known as hyperglycemia. Without proper diabetes care, serious problems can happen. But, with correct treatment like insulin shots, eating right, and exercising, people with Type 1 Diabetes can control their condition and stay healthy.
It’s crucial to spot the diabetes symptoms early to avoid big health troubles. Symptoms, such as needing to pee a lot, being very hungry, and feeling tired, might differ between kids and adults. Paying close attention to these signs is important. Catching it early can help prevent serious issues like diabetic ketoacidosis (DKA).
Keep reading as we dive more into the details of Type 1 Diabetes. We’ll cover its causes, symptoms, risk factors, and how to best manage and care for it.
What is Type 1 Diabetes?
Type 1 diabetes is a serious health issue. It happens when the body’s immune system attacks insulin-making cells in the pancreas. Because of this, controlling blood sugar levels becomes difficult.
The Role of Pancreatic Beta Cells
Pancreatic beta cells make insulin, which is needed to control blood sugar. In type 1 diabetes, the immune system attacks these cells. This stops them from making enough insulin.
Insulin and Blood Sugar Management
Insulin is key for managing blood sugar since it helps glucose enter cells for energy. Without enough insulin, glucose stays in the blood. This leads to high blood sugar levels, known as hyperglycemia, which is dangerous over time.
Autoimmune Response
In autoimmune diabetes, the immune system wrongly sees pancreatic beta cells as threats. It attacks and destroys them. This mistake by the immune system affects the body’s ability to manage blood sugar. Catching this autoimmune response early is vital for taking care of type 1 diabetes.
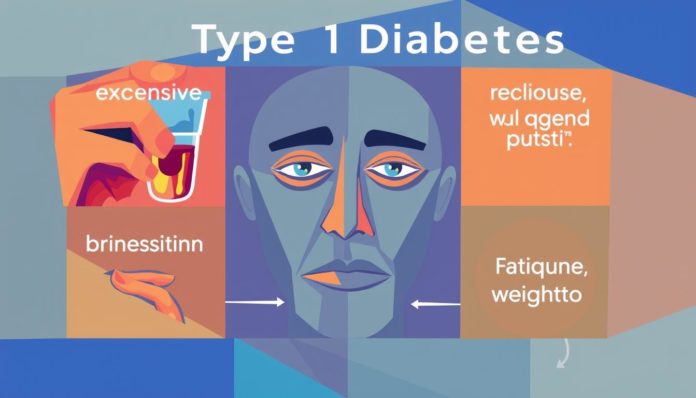
Symptoms of Type 1 Diabetes
Spotting Type 1 Diabetes signs early is key. Symptoms can surprise you, especially in kids. Knowing them helps manage the condition.
Common Symptoms in Children
Signs in kids often show up fast. Key symptoms in children cover:
- Frequent urination
- Extreme hunger
- Unexpected weight loss
- Irritability or mood changes
- Fatigue and weakness
Parents need to watch out and rush for medical help if they spot these signs.

Common Symptoms in Adults
Adults sometimes get wrongly diagnosed with Type 2 Diabetes. Their common symptoms are:
- Fatigue
- Blurry vision
- Increased thirst and frequent urination
- Sudden weight loss
- Persistent infections
Adults with these signs need to test for diabetes. It ensures they get the right treatment.
Recognizing Diabetic Ketoacidosis (DKA)
Diabetic Ketoacidosis is serious. It happens when the body makes too many ketones. Spotting DKA symptoms early is crucial:
- Nausea and vomiting
- Abdominal pain
- Rapid breathing
- Confusion or difficulty concentrating
- Fruity-scented breath
DKA needs quick medical help. Fast action and treatment can be lifesaving.
How Type 1 Diabetes is Diagnosed
Doctors diagnose Type 1 Diabetes using blood tests that check glucose levels and look for certain markers. These tests help confirm if someone has Insulin-dependent Diabetes. They also guide doctors in choosing the best treatment.
Blood Tests and Markers
For diagnosing, Diabetes Blood Tests are key. They check how the body handles blood sugar. An A1C Test shows the average blood sugar level over three months. This helps confirm diabetes. Tests for autoimmune antibodies are also crucial. They show if the immune system is attacking insulin-making cells.
Difference Between Type 1 and Type 2 Diabetes
It’s important to know if it’s Type 1 or Type 2 Diabetes. A C-peptide test checks if the pancreas makes enough insulin. With Type 1 Diabetes, insulin production is very low or not happening. But in Type 2, the body might make insulin but not use it well. Using Diabetes Blood Tests and testing for antibodies help decide the best treatment.
Understanding the Risk Factors
Type 1 Diabetes has several risk factors that can increase someone’s chance of getting it. Knowing these can help manage or even prevent the disease.
Genetic Predisposition
Our genes play a big part in our risk for Type 1 Diabetes. If you have a parent or sibling with it, your risk is higher. Scientists have found certain genes that contribute to this risk.
Environmental Triggers
Things around us can also trigger Type 1 Diabetes. This includes viral infections or exposure to certain pathogens. These can start the autoimmune process that leads to diabetes.
Age and Geography
Type 1 Diabetes is more common at specific ages, usually in kids or teens. Where you live affects your risk too.
People living away from the equator are more likely to get it. This shows that genes and environment both matter a lot.
Treatment Options for Type 1 Diabetes
Managing Type 1 Diabetes is all about keeping blood sugar at a safe level. Let’s look at the best ways to do this.
Insulin Therapy
Insulin Therapy is key for controlling Type 1 Diabetes. Patients may inject insulin several times a day or use an insulin pump. These approaches help keep blood sugar stable. There are different kinds of insulin, like rapid-acting and long-acting. Doctors tailor the insulin type and how it’s given based on what each patient needs.
Continuous Glucose Monitoring (CGM)
CGMs are a big step forward in Diabetes care. They show glucose levels in real-time. This helps people adjust their insulin dose more accurately. CGMs also warn if glucose levels go too high or low, helping avoid problems before they happen.
Insulin Pumps
Insulin Pumps are great for steady blood sugar control. They send insulin through a tiny tube under the skin. You can set the pump to give more or less insulin based on your daily needs. This method is often more effective than taking shots several times a day.
By using Insulin Therapy, CGMs, and Insulin Pumps together, people with Type 1 Diabetes can greatly improve their management of the condition. A plan that’s tailored for each person is essential for the best health results.
Importance of Blood Sugar Monitoring
Checking your blood sugar regularly is key to managing diabetes well. It allows people to choose wisely about their food, meds, and health. Blood glucose meters and CGM devices are great tools for this important task.
Using Blood Glucose Meters
Blood glucose meters are popular for monitoring blood sugar. They give quick results and don’t cost much. These devices need just a little blood from your fingertip. Here’s how to use them:
- Wash and dry your hands to ensure accuracy.
- Insert a test strip into the glucose meter.
- Prick your fingertip with the lancing device.
- Put the blood on the test strip.
- Wait for your blood sugar level to show up.
Benefits of Continuous Glucose Monitoring
CGM systems offer a bigger picture of sugar levels than blood glucose meters. Benefits of CGM include getting data in real-time. They also warn you if your sugar is too high or too low. This can help avoid danger and shows how food, activity, and meds affect sugar levels.
Here’s a comparison between blood glucose meters and CGM devices:
| Feature | Blood Glucose Meters | Continuous Glucose Monitoring |
|---|---|---|
| Cost | Less expensive | Costs more |
| Data Frequency | Shows single readings | Gives continuous real-time data |
| Alerts | No automatic warnings | Sends automatic alerts for high/low sugar |
| Trend Analysis | Offers limited insights | Provides deep analysis |
Using both blood glucose meters and CGM systems can greatly help people with diabetes. They get a better grip on their condition this way.
Managing Diet and Carbohydrate Intake
Managing your diet is key when you have Type 1 Diabetes. It’s crucial to grasp the role of Carbohydrate Counting in controlling blood sugar. Since carbs turn into glucose in your body, knowing how much is in your food lets you adjust your insulin correctly. This helps greatly in managing your diabetes diet and keeping your blood sugar in check.
To effectively add Carbohydrate Counting to your daily life, follow these steps:
- Consult with healthcare providers to develop a personalized meal plan.
- Learn to read nutrition labels to identify carbohydrate content accurately.
- Utilize digital tools or apps to track carbohydrate intake consistently.
- Adjust insulin doses based on the carbohydrate count to maintain balance.
- Regularly review and update your meal plan with your dietitian or doctor.
Working closely with your healthcare team can make a big difference. Creating a meal plan that’s just for you helps match your insulin doses with how many carbs you eat. This custom plan is key for improving your overall diabetes diet management.
| Food Item | Carbohydrate Content (g) |
|---|---|
| Apple (medium) | 25 |
| Bread (1 slice) | 15 |
| Cooked Pasta (1 cup) | 30 |
| Milk (1 cup) | 12 |
| Yogurt (6 oz) | 15 |
Knowing how many carbs are in your food is key. This table shows the carbs in common foods to aid in Carbohydrate Counting. With accurate counting, you can better manage your blood sugar. This highlights why good diabetes diet management is so important.
Exercise and Physical Activity
Exercise is key for those with Type 1 Diabetes. It not only helps keep blood sugar levels right but also boosts insulin sensitivity. Making physical activity a part of your daily life can greatly better your health.
Aerobic exercises and strength training play a big part in handling diabetes well. It’s important to keep a good balance between insulin doses, what you eat, and how much you move. Keeping blood sugar stable is a big goal. Plan ahead, check your sugar levels, and be ready to deal with low blood sugar to exercise safely.
Kids with Type 1 Diabetes may need more checks. Carbs may also need to change based on their age, size, and how active they are. This helps avoid big changes in blood sugar during exercise. It’s wise to talk to a health care team for advice on balancing diabetes and being active.
Here are tips for managing diabetes and exercise:
- Balance your insulin and carbs well.
- Check your blood sugar often.
- Always have snacks ready for low blood sugar.
Following these steps and sticking to a regular exercise plan makes managing diabetes easier. It also does wonders for your health.
Preventing and Managing Diabetes Complications
Living with Type 1 Diabetes requires always being on the lookout. Both short and long-term complications can greatly affect how well you live. By knowing and acting on these risks, you significantly lower the chance of severe health problems.
Short-Term Risks
Short-term issues usually come from quick changes in blood sugar. Hypoglycemia, or very low blood sugar, poses an immediate threat. With signs like dizziness and sweating, it demands quick action to prevent serious problems. Checking blood sugar often and having snacks like glucose tablets nearby are key.
Long-Term Risks
Not managing Type 1 Diabetes can lead to bigger health issues over time. Problems can include heart disease, kidney damage, and nerve damage. High blood sugar levels over time play a big part in these complications. That’s why regular health checks and a solid diabetes care plan are important.
Preventative Measures
To avoid diabetes complications, start with careful blood sugar monitoring and a healthy life. Exercise regularly, eat well, and follow your insulin treatment. Using tools like CGMs gives you instant blood sugar readings. Seeing your doctor regularly helps tailor prevention plans, keeping you healthy in the long run.
FAQ
What is Type 1 Diabetes?
Type 1 Diabetes, also known as Juvenile Diabetes, occurs when the immune system attacks the pancreas. This attack destroys cells that make insulin. Without enough insulin, the body can’t manage blood sugar levels properly.
What role do pancreatic beta cells play in Type 1 Diabetes?
Pancreatic beta cells make insulin, which is vital for allowing glucose to enter cells for energy. In Type 1 Diabetes, these cells are attacked by the immune system. This leads to a significant decrease in insulin production.
How does insulin help with blood sugar management in Type 1 Diabetes?
Insulin is key for controlling blood sugar by enabling glucose to enter cells for fuel. Without it, glucose stays in the blood, leading to high blood sugar levels and serious health issues.
What triggers the autoimmune response in Type 1 Diabetes?
The exact cause of the immune attack is unclear. Researchers think genes, environment, and possibly viruses play a part. These factors may initiate the immune attack on pancreas cells.
What are common symptoms of Type 1 Diabetes in children?
Children may show signs like needing to urinate often and feeling very hungry. They might also lose weight without trying and feel tired often. Catching these signs early is important for quick treatment.
What are common symptoms of Type 1 Diabetes in adults?
Adults can have symptoms like feeling tired, having blurry vision, needing to pee a lot, and unexpected weight loss. Sometimes it’s wrongly thought to be Type 2 Diabetes because it’s in adults.
What is Diabetic Ketoacidosis (DKA) and how can it be recognized?
DKA is a serious issue that happens when there’s not enough insulin and ketones build up in the blood. Signs include feeling sick to your stomach, throwing up, belly pain, breathing fast, and feeling confused. It requires quick medical help.
How is Type 1 Diabetes diagnosed?
Doctors diagnose it by checking blood for glucose levels, A1C, and antibodies. Tests like C-peptide and antibody tests separate it from Type 2 Diabetes.
What are the risk factors for developing Type 1 Diabetes?
Risk factors include genes, things in the environment, where you live, and your age. Having family members with it also increases your risk.
What treatment options are available for Type 1 Diabetes?
Treatment mainly involves taking insulin through shots or a pump. Using a Continuous Glucose Monitor (CGM), eating healthily, and exercising help too. The insulin type and method may differ for each person.
Why is blood sugar monitoring important for Type 1 Diabetes management?
Keeping a close eye on blood sugar is crucial. It lets you fine-tune insulin doses, meals, and activity. This way, you avoid dangerous blood sugar levels.
How do blood glucose meters and Continuous Glucose Monitoring (CGM) systems differ?
Glucose meters give fast blood sugar readings and are less expensive. CGM systems track glucose levels all the time, offering more detailed insights and warnings for high or low sugars.
How does diet impact Type 1 Diabetes management?
What you eat greatly affects blood sugar control. Counting carbs helps match insulin to food intake, so knowing the carb content in foods is crucial.
How does exercise benefit individuals with Type 1 Diabetes?
Exercise increases insulin’s effectiveness and helps keep blood sugars stable. It also improves overall health, making it important for managing diabetes.
What complications are associated with Type 1 Diabetes?
People with Type 1 Diabetes can face both immediate problems like low blood sugar and long-term dangers like heart disease. Staying on top of blood sugar and leading a healthy lifestyle are key to avoid these issues.