A Carotid-cavernous fistula, or CCF, demands careful observation in neuro-ophthalmology. It’s a vascular condition that needs a smart approach for management. It happens when there’s an unusual link between the carotid artery and the cavernous sinus. This affects the eyes and nerves.
Good care for this condition can really help patients do better. We’ll explore what causes CCF, how to spot it, and how to manage it well. Spotting it early and managing it effectively is key.
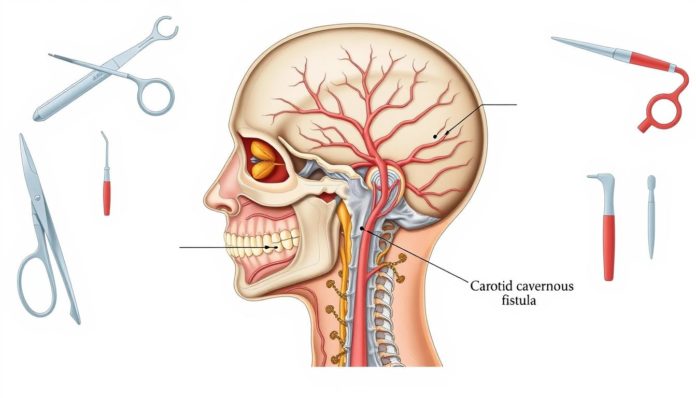
What is a Carotid-Cavernous Fistula?
A Carotid-Cavernous Fistula (CCF) is a health issue where the carotid artery wrongly connects to the cavernous sinus. The cavernous sinus is important because it contains nerves and blood vessels in the brain. Knowing what CCF is, its types, and how it looks inside the body helps in diagnosing and treating it.
Definition and Anatomy
The CCF definition includes an unusual link from the carotid artery to the cavernous sinus. This concern affects parts of the brain, specifically the internal and external carotid arteries. The cavernous sinus is next to the pituitary gland. This location is key due to many cranial nerves there, like the oculomotor and trochlear nerves.
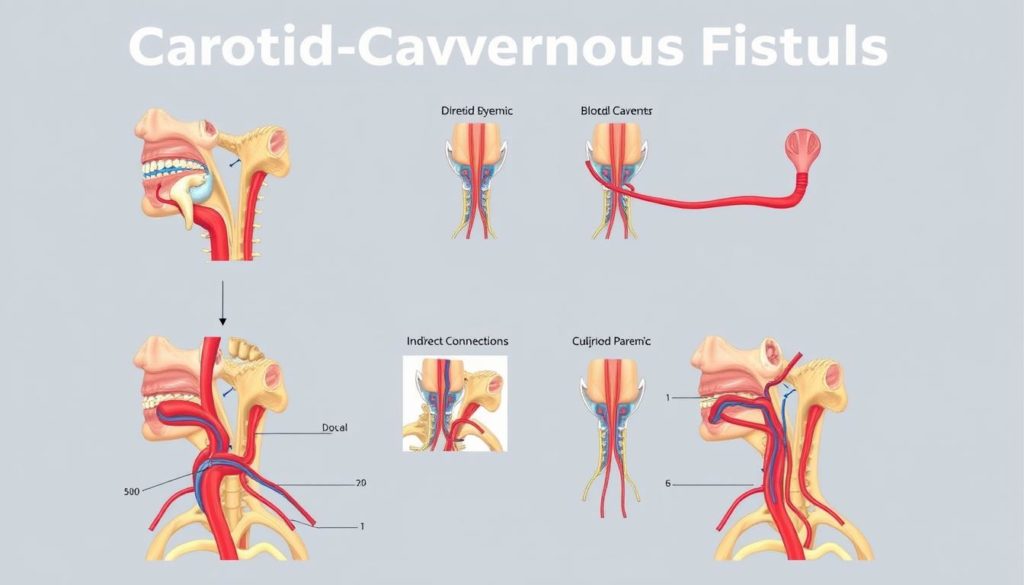
Types of Carotid-Cavernous Fistulas
Carotid-Cavernous Fistula types vary based on their cause and blood flow. Some happen because of an injury, while others occur on their own. They are also sorted by how the blood moves through them.
- Type A: Direct high-flow fistula involving the internal carotid artery.
- Type B: Indirect low-flow fistula through the meningeal branches of the internal carotid artery.
- Type C: Indirect low-flow fistula through the meningeal branches of the external carotid artery.
- Type D: Mixed high and low-flow fistulas with connections to both internal and external carotid arteries.
Understanding these types of Carotid-Cavernous Fistula is important for doctors. It helps them diagnose the condition correctly and pick the best treatment. Knowing how CCF affects the brain’s structure is crucial for giving patients the care they need.
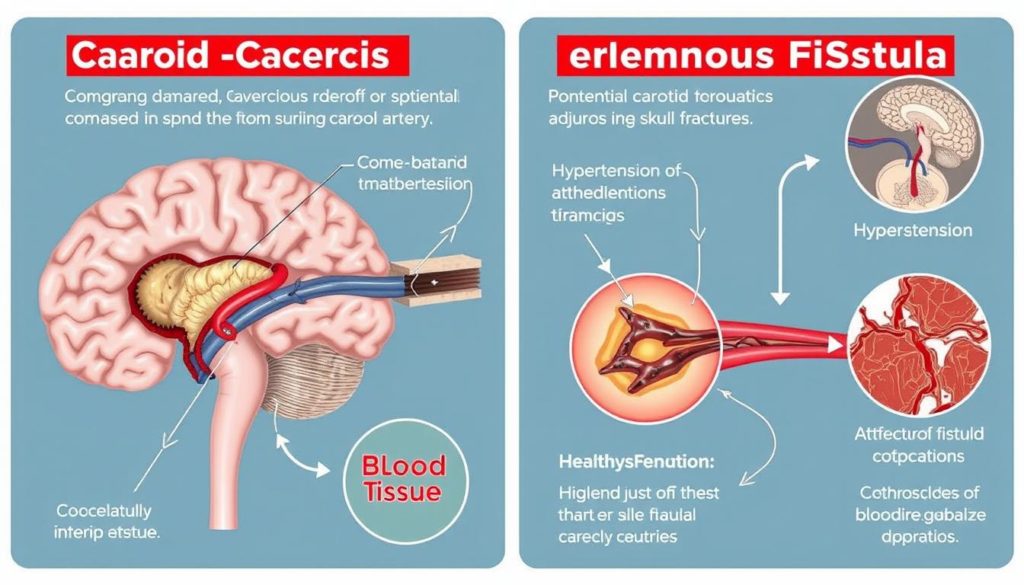
Causes and Risk Factors of Carotid-Cavernous Fistula
The CCF etiology falls into two main categories: traumatic and spontaneous. Each category has its own set of risk factors and causes. Knowing these can help with early diagnosis and treatment.
Traumatic Causes
A traumatic carotid-cavernous fistula usually happens after a serious head injury. This could be a hard hit to the head or a car crash. These incidents might tear the artery wall. This tear can create an abnormal link between the carotid artery and the cavernous sinus.
Iatrogenic damages during surgery near the brain, neck, or sinuses can also cause traumatic carotid-cavernous fistulas.
Spontaneous Causes
Spontaneous CCF risk factors are often linked to health problems or genetic issues. Aneurysms are one example. These are weak spots on a blood vessel that can burst and start a carotid-cavernous fistula.
Other spontaneous causes include conditions like Ehlers-Danlos syndrome, where arteries are naturally weak. This weakness makes it easier for an abnormal artery connection to happen on its own. People with high blood pressure or connective tissue diseases are also at risk.
| Cause | Trigger | Risk Factors |
|---|---|---|
| Traumatic | Head Injuries, Surgical Interventions | Motor Vehicle Accidents, Brain Surgeries |
| Spontaneous | Genetic Predispositions, Aneurysms | Ehlers-Danlos Syndrome, Severe Hypertension |
Symptoms of Carotid-Cavernous Fistula
Carotid-Cavernous Fistula shows different symptoms based on its type and how quickly it happens. A high-flow, direct fistula usually shows strong symptoms quickly. An indirect, low-flow fistula may show symptoms more slowly.
Acute Symptoms
When an acute CCF appears, symptoms come on fast. People with this type of CCF often have three main symptoms. These are proptosis, ocular bruit, and chemosis.
- Proptosis: This means the eye bulges out, a clear sign related to CCF.
- Ocular Bruit: This is when a rushing sound is heard in the eye.
- Chemosis: This is when there is swelling of the conjunctiva, showing signs of acute CCF.
It’s really important to get medical help right away to take care of these symptoms.
Gradual Onset Symptoms
Indirect or low-flow CCFs don’t show signs as quickly. They develop over time. Some symptoms to look out for include:
- Eye Bulging: The eye slowly starts to stick out more, a serious symptom of CCF.
- Congestion: The eyes get red and bloodshot.
- Occasional Headaches: Headaches often happen with a gradual symptom show of Carotid-Cavernous Fistula.
If the symptoms come on slowly, it could lead to a late diagnosis and treatment of CCF. This makes being aware and getting diagnosed quickly very important.
Knowing these symptoms early makes treating and managing them better. It’s crucial to seek medical advice when these symptoms appear for the best care.
| Symptoms | Acute CCF | Gradual Onset CCF |
|---|---|---|
| Proptosis | Rapid | Progressive |
| Ocular Bruit | Present | Usually Absent |
| Chemosis | Prominent | Mild or Absent |
| Headaches | Occur | Frequent |
| Eye Congestion | Severe | Noticeable |
How is Carotid-Cavernous Fistula Diagnosed?
Getting the right diagnosis for Carotid-Cavernous Fistula (CCF) is very important for treatment. It requires careful physical checks and special imaging tests.
Physical Examination
Diagnosis starts with a detailed physical exam. Doctors look at:
- Reviewing patient history
- Conducting a visual inspection for ocular abnormalities
- Utilizing tonometry to measure intraocular pressure
- Applying Doppler ultrasonography to assess blood flow in the carotid artery
Imaging Tests
When physical exams suggest problems, imaging tests offer more detail. They are vital to confirm a CCF diagnosis and figure out its extent. Widely used imaging tests include:
| Imaging Test | Description |
|---|---|
| CT Scan | Helps visualize the bones and blood vessels |
| MRI | Provides detailed images of soft tissues |
| CTA (CT Angiography) | Combines a CT scan with an injection of a contrast material to show blood flow |
| MRA (Magnetic Resonance Angiography) | Uses magnetic fields and radio waves to visualize blood vessels |
| Cerebral Angiography | The definitive test, using X-ray and dye to map blood flow and detect abnormalities |
A combination of a thorough exam and imaging tests enables a correct diagnosis. This way, doctors can plan the best treatment for Carotid-Cavernous Fistulas.
Treatment Options for Carotid-Cavernous Fistula
The treatment approach for CCF varies by the fistula’s severity and details. Tailoring the treatment to each patient is key. This ensures the highest success rate and the least complications.
Conservative Management
For those with low-risk or small fistulas, conservative management may be the best route. This method includes:
- Compression therapy, where patients apply pressure to reduce blood flow and encourage natural closure.
- Regular monitoring to observe any changes or developments in the condition without immediate invasive intervention.
Endovascular Intervention
Endovascular intervention CCF is ideal for more severe or symptomatic cases. It’s favored for its effectiveness and minimal invasiveness. Intervention techniques may involve:
- Embolization with coils or liquid embolic materials to stop abnormal blood flow.
- Stent placement to support artery walls and ensure proper blood circulation.
Each treatment is chosen after considering the fistula’s traits, patient health, and desired outcome.
Role of Neuro-Imaging in CCF Diagnosis
Neuro-imaging is key for spotting and treating Carotid-Cavernous Fistula (CCF). It lets doctors see how severe the CCF is. This helps them make a good plan for treatment.
CT and MRI
CT scans and MRIs are important for looking at CCF without surgery. A CT scan for CCF shows important changes like a swollen Superior Ophthalmic Vein (SOV). It gives doctors useful info about the illness. An MRI brings out details in soft tissue better. This makes it easier to see if there’s vein swelling. It also shows how much the fistula is affecting nearby parts.
Angiography
Angiography is the best way to figure out if it’s CCF. It gives a clear picture of blood vessels. This shows exactly how the fistula is and where it’s draining. Angiography CCF diagnosis is more hands-on but very clear. It’s crucial for planning surgery and choosing the right treatment.
| Imaging Method | Advantages | Limitations |
|---|---|---|
| CT Scan | Quick, Noninvasive, Good visualization of bony structures | Radiation exposure, Less soft tissue contrast |
| MRI | Excellent soft tissue contrast, No radiation, Detailed cross-sectional images | Longer time, More expensive, Not suitable for all patients |
| Angiography | High-resolution vessel images, Precise diagnosis, Essential for surgical planning | Invasive, Risk of complications, Requires contrast dye |
Each neuro-imaging method has its pros and cons. Picking the right one depends on the patient’s needs. Together, these methods give doctors a full view. This is key for taking care of Carotid-Cavernous Fistulas well.
Complications Associated with Carotid-Cavernous Fistula
Carotid-cavernous fistula (CCF) is a condition that poses serious risks. It happens when the carotid artery wrongly connects with the cavernous sinus. Knowing the risks is key for catching it early and managing it well.
Ophthalmoplegia
One key complication of CCF is ophthalmoplegia. This condition leads to eye muscle weakness or paralysis. It makes moving the eyes hard, often causing double vision and hurting life quality. Quick help is key to avoid lasting eye damage.
A study by the National Center for Biotechnology Information says knowing about CCF can really help patients. It can make outcomes better.
Cerebral Infarction
Cerebral infarction is another serious problem from CCF. Abnormal blood flow can cause a block. This block stops oxygen from getting to parts of the brain, killing tissue. This danger calls for fast medical help to avoid lasting brain harm.
Here’s a table that compares common CCF complications:
| Complication | Symptoms | Management |
|---|---|---|
| Ophthalmoplegia | Eye muscle paralysis, double vision | Surgical or endovascular intervention, supportive therapy |
| Cerebral Infarction | Sudden severe headache, neurological deficits | Immediate medical intervention, anticoagulation therapy |
So, it’s really important for CCF patients to know about ophthalmoplegia and cerebral infarction risk. Knowing these risks helps get the right medical care quickly. This can prevent lasting damage.
Prognosis and Recovery
The CCF prognosis is typically good, especially with early help. Most symptoms start to lessen within a few hours to days after treatment. But, everyone’s recovery from Carotid-Cavernous Fistula is different, depending on their situation and the treatment they get.
Recovery time can range from a few weeks to several months. The severity of the condition and the treatment type matter a lot. Regular check-ups and personalized rehab plans are important. They help speed up recovery and lower the chance of coming back, which doesn’t happen often.
Here’s what you might expect for recovery times and results:
| Recovery Stage | Time Frame | Symptoms |
|---|---|---|
| Immediate Post-Treatment | Hours to Days | Decrease in acute symptoms |
| Short-Term Recovery | Weeks | Gradual improvement in overall function |
| Long-Term Recovery | Months | Complete symptom resolution in most cases |
Knowing what to expect from CCF recovery helps patients and their caregivers get ready. It makes sure they have the right support and resources for a successful recovery from Carotid-Cavernous Fistula.
Preventive Measures and Patient Education
Stopping CCF before it starts needs the right knowledge and actions. We will cover three main points for teaching patients about Carotid-Cavernous Fistula.
Avoiding Trauma
Staying away from head and neck injuries is key to stopping CCF. It’s important to always buckle up, wear helmets and guards during sports, and watch out for trip hazards. These steps greatly lower the chances of getting a Carotid-Cavernous Fistula. Teaching patients about these safety steps is crucial.
Managing High Blood Pressure
High blood pressure can lead to CCF. So, controlling it with lifestyle tweaks, a balanced diet, exercise, and following your doctor’s advice is vital. Doctors should make sure their patients know how to keep their blood pressure in check. This will help avoid CCF problems.
Regular Follow-ups
Checking in with your doctor often is important for catching CCF early. These visits help spot small problems before they get bigger, leading to better outcomes. Making these check-ups a regular part of your care is key, along with learning all you can about CCF.
| Preventive Measure | Detail |
|---|---|
| Avoiding Trauma | Use protective gear, be cautious in risky environments, and adopt safe practices. |
| Managing High Blood Pressure | Implement lifestyle changes, adhere to medical advice, and monitor regularly. |
| Regular Follow-ups | Schedule and attend routine check-ups to monitor health status consistently. |
Living with Carotid-Cavernous Fistula
Living with CCF may seem tough, but it’s doable to live well. Start by closely following your treatment. This means going for regular check-ups and taking your medicine as told. You might also need some surgeries to help manage CCF. It’s key to always talk with your doctors to catch any issues early.
To manage daily life, focus on reducing stress and staying healthy. Eat well, get approved exercise, and be careful to avoid injuries. Adjusting your home and work for better lighting and less screen time helps too. These changes help protect your vision and brain health.
Learning about CCF gives you control. Understanding your condition helps you stick to your treatment plan better. Joining a support group offers emotional and practical help from those who know what you’re experiencing. With the right knowledge and support, you can tackle CCF and enjoy a good life.
FAQ
What is a Carotid-Cavernous Fistula (CCF)?
A Carotid-Cavernous Fistula (CCF) is when the carotid artery and a big vein at the brain’s base mistakenly connect. It can cause different symptoms because the blood flow changes near nerves and veins.
What causes a Carotid-Cavernous Fistula?
CCF may happen after a head injury or surgery. It can also come on its own from genetic issues, aneurysms, or weak arteries.
What symptoms are associated with Carotid-Cavernous Fistula?
Symptoms of CCF can start suddenly or slowly. Rapid symptoms include an eye popping out, noisy blood flow, and swollen eye tissue. Slow symptoms cover eye puffiness, popping out, and sometimes headaches.
How is Carotid-Cavernous Fistula diagnosed?
Doctors check for CCF with a deep physical exam and imaging tests. Tests like CT, MRI, and angiography show the unusual blood flow.
What treatment options are available for CCF?
Treatment ranges from simple compression therapy to complex surgeries using coils or glues. Surgery is often the best choice.
What role does neuro-imaging play in diagnosing CCF?
Neuro-imaging, such as CT and MRI, shows signs of CCF without surgery. It helps find issues like a swollen Superior Ophthalmic Vein. Angiography then details the fistula’s type and flow pattern.
What are some complications associated with Carotid-Cavernous Fistula?
Complications can include eye muscle paralysis, vision loss, blocked eye arteries, and brain strokes. Quick treatment is key to avoid lasting eye or brain damage.
What is the prognosis and recovery like for CCF?
With the right treatment, CCF has a good outcome. Symptoms often improve in hours to days. Full recovery may take weeks to months. Cases coming back are rare.
How can Carotid-Cavernous Fistula be prevented?
Prevent CCF by avoiding head injuries, controlling blood pressure, and having regular check-ups. Teaching about risks and quick action for serious symptoms is vital.
What lifestyle changes are recommended for living with CCF?
Living with CCF means managing symptoms, following treatment, and adjusting lifestyle to reduce vascular stress. Staying in touch with doctors is essential for the best care.