Imagine looking through a camera lens that’s always blurry. It’s like trying to clean it, but the smudge won’t go away. This is what life feels like for those with refractory uveitis. It’s a constant battle with an eye inflammation that clouds their vision and dims their hope. Many follow their treatments closely, yet find no relief. They experience frustration as clear vision and comfort become elusive.
Yet, this story isn’t just about struggle. It’s also about coping with uveitis during hard times and discovering new ways to take control of one’s story. For those dealing with managing recurrent uveitis, finding hope and comfort often means exploring new solutions. It’s about changing the story, becoming resilient, and relying on a supportive community.
Soon, we will explore a variety of strategies and support systems. They are meant to help those with persistent uveitis navigate through this foggy condition when standard treatments fail. Knowledge and understanding can be powerful allies. They help many find some clarity. Join us to learn how to live with this challenging condition without letting it define you.
Understanding Uveitis: A Comprehensive Overview
What is uveitis? Many people ask this when they feel severe eye pain or get this diagnosis. Uveitis is a group of inflammatory diseases that make the eye swell and damage its tissues. This can cause vision loss ranging from minor to extreme if not treated right. We’ll cover the types, causes, symptoms, and how to manage uveitis.
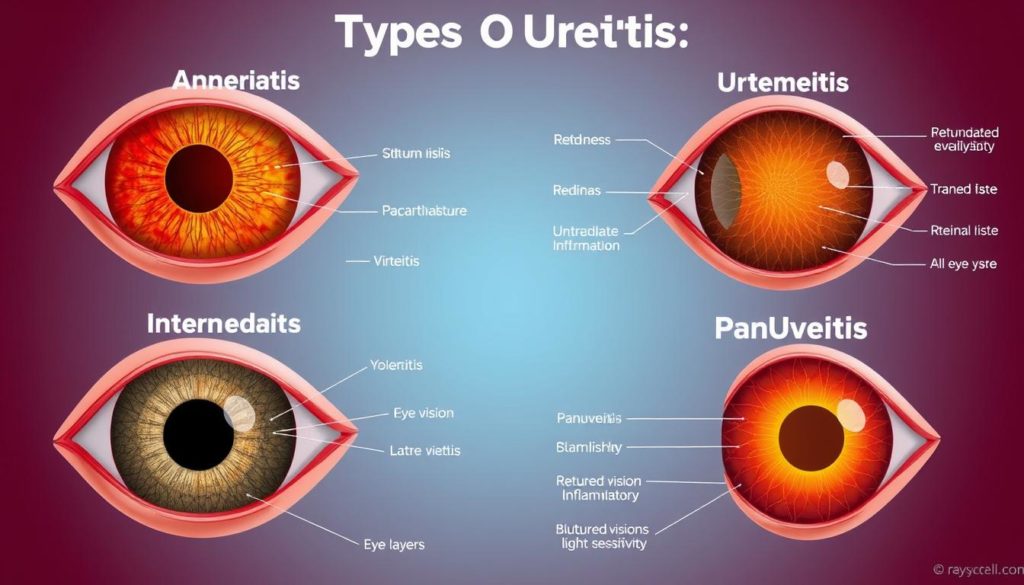
Handling uveitis therapy and uveitis management means understanding its variety. It’s classified by the eye part affected: anterior, intermediate, posterior, or panuveitis, affecting all layers. Symptoms can include redness, pain, blurry vision, and sensitivity to light, depending on the type.
Uveitis causes vary as much as the types. Triggers include autoimmune diseases, infections, or toxins, but often the cause is unknown. This unknown factor makes uveitis therapy a challenge, requiring personalized treatment for effectiveness.
- Autoimmune Disorders: Conditions like sarcoidosis, rheumatoid arthritis, and ankylosing spondylitis can lead to uveitis.
- Infections: It can be caused by viruses, bacteria, fungi, or parasites. Examples are herpes simplex virus and tuberculosis.
- Toxic Exposure: Certain chemicals or toxins might also trigger it, though less common.
Uveitis treatment aims to stop inflammation, ease pain, prevent more damage, and fix any vision loss. Treatments may include steroids for inflammation or antibiotics for infections. In long-term or severe cases, treatments might also involve immunosuppressive drugs or biologic therapies as part of a broader uveitis therapy strategy.
| Type of Uveitis | Common Symptoms | Potential Causes |
|---|---|---|
| Anterior Uveitis | Redness, pain, blurred vision | Mostly linked with autoimmune diseases |
| Intermediate Uveitis | Floaters, blurred vision | Often connected to systemic diseases |
| Posterior Uveitis | Vision loss, floaters | Caused by infections or cancer at times |
| Panuveitis | All the above symptoms | Sometimes the cause is unknown |
This table helps us grasp uveitis management complexities. It shows why different cases need unique treatment plans within uveitis therapy. Knowing the specific type and cause is key to picking the best treatment, which significantly helps lessen this condition’s effects on vision and daily life.
Evaluating Why Uveitis Treatments May Not Work
Finding out why uveitis therapy fails is key to helping patients. We look into patients’ past health, how their immune systems work, and issues with medicine working well and being tolerated.
Analyzing Patient Histories
A patient’s past health can greatly affect uveitis treatment. By looking closely, we might spot trends that help us understand why uveitis comes back. This helps make treatments better.
Exploring the Role of Immune System Variability
Everyone’s immune system works a bit differently. This affects how well uveitis treatments work. Knowing these differences helps us figure out why treatments don’t work for some and adjust accordingly.
Assessing Medication Efficacy and Tolerance
Not all patients do well with the same uveitis treatments. It’s critical to see how well medicines work and if patients can handle them.
Improving uveitis treatments with these insights can cut down on relapses. It can make life better for those affected.
| Factor | Impact on Treatment Success | Notes |
|---|---|---|
| Patient History | High | Prior health conditions influence treatment response |
| Immune System Variability | Moderate to High | Different immune responses can change how well treatments work |
| Medication Tolerance | Moderate | How well a treatment is handled can limit options |

When Uveitis Treatment Fails: What Next?
Finding out your uveitis treatment didn’t work can be tough. We’ll cover what to do after a uveitis treatment fails and look at other ways to handle uveitis.
- Reevaluation of your diagnosis to confirm the type and cause of uveitis.
- Consultation with a specialist in uveitis to discuss advanced treatment options.
- Investigation into underlying systemic conditions that may affect treatment outcomes.
After the initial medical steps, it’s essential to be proactive. Here are useful steps and options to explore:
- Intensified Monitoring: Regular check-ups can spot changes early, helping to avoid major issues.
- Adjustment of Therapeutic Plans: Your treatment may need changes based on new findings, including new meds or methods.
- Integration of Lifestyle Modifications: Adding changes like diet, exercise, and stress control can help manage symptoms.
- Exploration of Surgical Options: Surgery might be needed if other treatments can’t reduce inflammation.
Talking about other ways to manage uveitis with your doctor is key. It’s important to know the pros and cons of each choice.
“Taking a full and flexible approach to manage uveitis can control the disease and better your life.”
Knowing about what to do if uveitis treatment fails is crucial. Being informed lets you make smart choices for your health.
Alternative Medical Therapies for Uveitis
Exploring alternative medical therapies gives new hope to those struggling with Uveitis. This is especially true for patients where standard treatments haven’t worked. We’ll look into three hopeful areas: off-label drug use, biologic medications, and the promise of experimental treatments.
Investigating Off-Label Drug Use
Off-label uveitis therapy has become a valid choice for many despite its risks. These therapies aren’t initially approved for uveitis. They’re considered when usual treatments fail. Off-label use includes drugs that can effectively regulate the immune system, even though they’re meant for other conditions.
Prospects of Biologic Medications
The arrival of biologic medications for uveitis is a major advancement. Biologics target specific parts of the immune system involved in inflammation. This precision therapy could greatly enhance life quality. Their use undergoes careful evaluation to match compatibility and reduce side effects.
The Potential of Experimental Treatments
Joining clinical trials for experimental treatments for uveitis opens doors to innovative therapeutic options. These are the latest in medical research, presenting fresh methods that might become standard in the future.
| Treatment | Target | Phase |
|---|---|---|
| Anti-TNF Therapy | Inflammatory pathways | Phase II |
| Interleukin Inhibitors | Immune modulation | Phase III |
| Gene Therapy | Molecular regulation | Pre-Clinical |
Lifestyle Adjustments to Manage Uveitis Symptoms
Making some lifestyle changes for uveitis can really help in managing life with uveitis. Think about eating better, moving more, and stressing less. Let’s look into how these changes can make a big difference in improving uveitis symptoms naturally.
- Dietary modifications: Incorporating anti-inflammatory foods such as leafy greens, nuts, and fatty fish can reduce inflammation that exacerbates uveitis symptoms.
- Consistent exercise: Engaging in regular moderate activity like walking or swimming helps control overall inflammation and boosts immune system function.
- Stress reduction techniques: Practices like yoga, meditation, and mindfulness are crucial for lowering stress, which might trigger or worsen symptoms.
| Lifestyle Factor | Benefits for Uveitis | Recommended Activities |
|---|---|---|
| Diet | Reduces internal inflammation | Anti-inflammatory diet plans |
| Exercise | Boosts immune system health | 30 mins/day of moderate aerobic activity |
| Stress Management | Decreases flare-ups frequency | Regular meditation or yoga sessions |
Adopting these lifestyle changes for uveitis is key in managing life with uveitis. It’s all about finding a good balance. This balance is crucial for feeling better and tackling uveitis challenges head-on.
Integrative Approaches to Managing Recurrent Uveitis
For those dealing with recurrent uveitis, combining traditional and holistic health methods can be life-changing. This approach brings together medical treatments and whole-body health practices. It puts a strong focus on nutritional strategies for uveitis.
Incorporating Nutritional Strategies
Eating right plays a crucial role in controlling inflammation, which causes uveitis flares. Adding certain nutrients to your diet can help manage these symptoms. Omega-3 fatty acids in fish and flaxseeds, along with antioxidants in colorful fruits and veggies, are essential. They help the immune system react better, reducing eye irritation and swelling.
Benefits of Holistic Health Practices
Looking into holistic health and uveitis reveals many advantages. Yoga, meditation, and acupuncture do more than ease stress. They might also make uveitis flare-ups less common by boosting overall health. These practices aim for a mind-body balance, promoting relaxation and fighting inflammation.
Learning to include these nutritional and holistic methods in your day-to-day life is a hopeful path for those with recurrent uveitis. It not only helps manage the condition but also enhances life quality.
Understanding the Complications of Uveitis
Uveitis is an inflammation in the eye that can cause immediate symptoms and long-term issues. It’s key to learn about these problems for better health management. This text explores the long-term effects of uveitis and health risks linked with this condition.
Recognizing Long-Term Effects on Vision
Not managing chronic uveitis well can lead to serious vision problems. Issues like cataracts, damage from glaucoma, or a detached retina can result. These are severe issues that can lead to a big loss in vision. The term complications of uveitis covers any problem caused by the initial inflammation. This shows why quick and effective treatment is vital.
Addressing Associated Health Risks
Uveitis can also signal other health issues beyond eye concerns. For instance, it may be linked to autoimmune diseases like rheumatoid arthritis or lupus, bringing extra health challenges. Knowing about these links helps in treating not just uveitis but the whole body.
| Complication | Possible Causes | Impact on Vision |
|---|---|---|
| Cataracts | Long-term inflammation | Potentially severe vision loss |
| Glaucoma | Increased eye pressure due to inflammation | Gradual loss of peripheral vision |
| Retinal Detachment | Lingering inflammation leading to retinal tears | Immediate and severe vision loss, potentially permanent |
Emotional and Mental Health Support for Uveitis Patients
Chronic illnesses like uveitis impact both body and mind. Engaging in mental health support for uveitis helps buffer against psychological strains. This section explores supports for those managing uveitis while wanting to stay psychologically well.
Understanding and coping with chronic uveitis emotionally is key to overall wellness. Patients often feel uncertain and frustrated. These feelings can lead to stress affecting their life quality. It’s critical to address emotional issues as diligently as physical symptoms.
- Counseling: Professional therapists help patients process feelings of anxiety, depression, or stress from chronic conditions.
- Support Groups: Connecting with others who face similar challenges offers mutual understanding and support. These groups provide emotional encouragement and practical advice for managing life with uveitis.
- Stress Reduction Techniques: Mindfulness meditation, yoga, and guided imagery can lessen stress and boost mental health.
Moreover, using emotional coping strategies daily can lessen uveitis’s psychological effects. It also aids in following medical treatments better and improving health outcomes. Individuals should regularly seek mental health support for uveitis. Healthcare providers should include these services in management plans.
“Acknowledging the psychological side of chronic illness is as important as treating its physical symptoms.” – Health Expert on Chronic Disease Management.
Maintaining a balanced life with uveitis is possible with proper support and coping methods. This highlights the need for care plans that include mental health support.
Dealing with Uveitis in Children and Adolescents
Treating uveitis in children is different from treating adults. Kids need care that meets both their medical and emotional needs. Pediatric uveitis management must focus on these special considerations.
Special Considerations for Pediatric Patients
Kids are not just smaller versions of adults. Their uveitis treatment must be designed for them. Specialists work hard to balance treatment effects with the child’s growth. This balance is key to protect their development.
Support Systems and Resources for Families
Family support for uveitis is key in managing the disease in kids. Families help by following treatment plans and watching for side effects. There are support groups, educational materials, and counseling services for these families.
- Informational sessions and workshops to educate families about uveitis
- Support groups that provide a platform for sharing experiences and tips
- Access to pediatric counselors or psychologists familiar with chronic illnesses
Good pediatric uveitis management and family support for uveitis reduce the disease’s impact. This helps children and families have better health outcomes and live better lives.
Exploring Surgical Interventions When Other Treatments Fail
When other treatments do not work, surgical interventions for uveitis might be necessary. This part looks into surgeries and new advances in ophthalmic surgery for uveitis. It gives hope to those fighting this tough condition.
Assessing the Risks and Benefits of Surgery
Thinking about surgery for uveitis means weighing its risks and benefits. Surgery can greatly help and protect the eye, but has risks like infection and complications from anesthesia. Talking thoroughly with doctors is key to a wise choice.
Recent Advances in Ophthalmic Surgical Techniques
New technologies have improved ophthalmic surgery for uveitis success rates. Minimally invasive methods and better imaging help surgeons be more accurate. These advances make surgery less tough on patients and lead to better results.
The Impact of Uveitis Therapy on Everyday Life
Living with uveitis means facing several challenges. These include how uveitis changes daily life, impacting work and personal moments. People with uveitis often change their lives to handle symptoms and treatment side effects.
Managing Work and Social Activities
Dealing with uveitis at work can be hard. Symptoms that change can affect work performance, leading to changes in work settings and duties. People might need to adjust lights, take breaks often, and use special visual tools. Also, uveitis can make social life tough because tiredness and discomfort can decrease socializing.
Navigating Healthcare Systems and Insurance
Navigating uveitis healthcare and insurance is tricky for patients. It’s hard to understand insurance and healthcare options. Patients need to research to find out what treatments are insured and how to get them.
Here’s a table showing common issues uveitis patients face with healthcare and insurance, and helpful strategies:
| Challenge | Strategy |
|---|---|
| High medication costs | Seek assistance programs and generic alternatives |
| Limited insurance coverage for specialized treatment | Consult with healthcare providers for necessary documentation to support claims |
| Difficulty scheduling timely appointments | Utilize patient portals for quicker communication and appointment setting |
| Lack of understanding of insurance benefits | Engage in consultations with insurance specialists |
The main goal for those battling uveitis is keeping a good quality of life. This means managing health well and staying active in work and social circles. By being proactive in healthcare and work adjustments, the negative effects of uveitis on everyday life can be lessened.
Second Opinions: When to Seek Further Medical Advice
When dealing with uveitis, it’s wise to consider a second opinion. Seeking second opinions for uveitis helps evaluate all treatment options. This is critical when initial treatments fail or symptoms get worse.
Knowing when and how to seek further advice can greatly impact your health journey. Here are the main points to keep in mind:
- Identifying the Need for a Second Opinion: It’s key if your symptoms don’t improve or get worse. This may mean your diagnosis or treatment plan needs another look.
- Choosing the Right Specialist: Find a specialist who knows a lot about uveitis. They might find new ways to handle your condition.
- Preparing for Your Appointment: Bring all your medical info, test results, and medication list. This gives the new doctor a full picture of your health and treatment.
Knowing the second doctor’s expertise is crucial. They should offer the latest and most relevant advice on uveitis.
| Benefits of Seeking a Second Opinion | Impact on Uveitis Management |
|---|---|
| New diagnostic insights | Potential for more targeted treatment |
| Revision of existing treatment plans | Improvement in symptom management |
| Introduction to new or experimental treatments | Opening avenues for better outcomes |
The aim of seeking second opinions for uveitis is to make sure you’re fully informed. This helps you make better health decisions for better results.
Natural and Home Remedies: Do They Help with Uveitis?
Many patients are looking at natural remedies for uveitis and home treatments for uveitis. They want to add these to their usual medical care. The move toward holistic methods shows we need to think about their role and success.
Evaluating the Effectiveness of Herbal Treatments
People around the world use herbal treatments for uveitis as softer options compared to drugs. Turmeric, for example, is famous for its ability to fight inflammation. Some studies and stories from people suggest herbs might help with mild uveitis.
Mind-Body Therapies and Their Role in Symptom Management
Yoga and meditation are good home treatments for uveitis too. They lower stress which can make chronic uveitis worse. Adding these practices into daily life can ease both physical symptoms and the stress of having an ongoing eye problem.
Even though natural remedies for uveitis and herbal treatments for uveitis seem promising, they’re best used with doctor-approved treatments. Talking to a healthcare provider is crucial before trying anything new to ensure it’s safe.
Staying Informed: The Importance of Ongoing Research
The medical world is always changing, especially for eye conditions like uveitis. Ongoing research for uveitis is key to finding new and better treatments. Keeping up with the latest findings is very important for anyone with this condition. Staying informed about uveitis treatments allows people to make good choices for their care. It also helps them work better with their doctors.
Learning about uveitis never stops because the knowledge around it is always growing. It’s important to look for reliable information and study results. Being part of, or following, clinical trials can offer early access to new treatments.
- Access to cutting-edge treatments
- Opportunities to contribute to medical research
- Enhanced understanding of condition management
Getting involved in ongoing research for uveitis brings patients, doctors, and researchers closer. This teamwork approach helps fight uveitis more effectively.
Staying informed about uveitis treatments means patients can keep up with new treatment changes. They’ll be ready to talk about new trials or therapies that might help them. This is crucial for their future health and life quality.
Taking time to learn about the latest in uveitis research and treatment can change your health journey. It leads to a much better outcome for your condition.
Final Thoughts: Empowerment Through Knowledge and Support
Dealing with uveitis is tough, from the first signs to treatment plans. Yet, knowing all about it can be your power. Through learning, you become able to make smart choices. You can also communicate well with doctors.
Support is key in fighting uveitis. It’s huge. Finding those who get what you’re going through is vital. Experts and resources can help too. This support lightens the emotional load and shows new treatment paths. Being in a community boosts your empowerment.
Empowerment is a journey. It means keeping up with new info and finding strong support networks. Let this guide help you stay strong and informed. Together, we face the challenges of uveitis with hope and strength.
FAQ
What coping strategies can I use when my uveitis treatment fails?
When uveitis treatment doesn’t work, different actions can help. Look into new medical options or join a clinical trial. Changing how you live, reducing stress, and finding support are key. This helps improve life with tough-to-treat uveitis.
What are the common reasons why uveitis treatments may not work?
Uveitis treatments fail for various reasons. It might be how your body responds or how you handle the medication. To find the cause, doctors often revisit your medical history. Understanding why can guide the next steps.
When should I consider alternative strategies for uveitis management?
If uveitis keeps coming back or treatments fail, think about other options. This might mean trying different drugs or joining a trial. Staying proactive is important to manage this condition.
How can lifestyle adjustments help manage uveitis symptoms?
Changing your lifestyle can ease uveitis symptoms. Eat anti-inflammatory foods and exercise to lower stress. Getting enough sleep can also prevent flare-ups. Quit smoking and limit screen time for extra benefits.
Can integrative approaches help with managing recurrent uveitis?
Yes, combining traditional and complementary treatments helps with recurring uveitis. Eating right and trying things like acupuncture or meditation can support your health. These may lessen how often uveitis flares up.
What complications should I be aware of with chronic uveitis?
Chronic uveitis might lead to serious eye issues like cataracts or glaucoma. It could even cause vision loss. Uveitis also raises the risk of infections. Watch for vision changes or eye pain and talk to your doctor.
Are there emotional and mental health resources available for individuals with uveitis?
Many resources address the mental effects of uveitis. Counseling, support groups, and online forums can help. Organizations like the American Uveitis Society offer support. It helps to connect with those who understand your situation.
What should I know about uveitis in children and adolescents?
Kids and teens with uveitis need special care. Their treatment may differ, and side effects must be watched. Families should seek support from specialists and groups focusing on young patients.
When should I consider surgical interventions for uveitis?
Surgery for uveitis is an option when other treatments don’t work or complications develop. Make this decision with a specialist. They’ll help weigh the risks and benefits.
How does uveitis therapy affect everyday life, and what can be done to manage these impacts?
Uveitis treatment touches on work, social life, and finances. Be honest with your employer and understand your insurance. Also, focus on self-care and seek support from social workers or advocates.
When is it appropriate to seek a second opinion for uveitis?
Get a second opinion if you’re unsure about your diagnosis or treatment isn’t working. Especially before considering surgery. Look for a specialist with a lot of experience in uveitis.
Are there any natural or home remedies that help with uveitis?
Some find comfort in herbal remedies and mind-body therapies. These should be used carefully. Always talk to your doctor before trying new therapies to make sure they fit your needs.
Why is it important to stay informed about ongoing research for uveitis?
New research can introduce groundbreaking treatments for uveitis. Being updated allows you to make better choices about care. It also opens doors to clinical trials offering new therapies.
How can patients feel empowered in managing their uveitis?
Understanding uveitis, participating in your care, and building support are key to empowerment. Stay current on treatments, work closely with your doctors, and connect with fellow patients.


