Imagine the eye as a universe of its own, full of important layers and structures. Now think about a disturbance in this universe—like sudden redness, pain, or blurry vision. These signs could point to uveitis, an inflammation dangerous to both vision and the eye’s balance. As we dive into What Is Uveitis?, we learn about a condition that can secretly damage one’s sight, often leaving people searching for answers in the midst of confusion.
Understanding uveitis symptoms can be tricky. Symptoms like redness, light sensitivity, and poor vision may seem small at first but can signal serious inflammation. Since vision is so critical, knowing about uveitis is key.
Yet, there’s still hope as new uveitis treatment options are found, bringing relief and the chance for recovery. This article will light the way through the challenges of uveitis. It offers a detailed guide to recognize, tackle, and manage this mysterious eye condition. Join us in uncovering the complexities of uveitis and finding ways to protect our most precious sense.
What Is Uveitis?
Have you ever wondered about Uveitis and its effects on eye health? Uveitis is not just a simple eye problem. It’s an inflammation impacting parts of the eye, mainly the uvea. The uvea plays a big role in seeing properly. Inflammation here can cause much discomfort and serious vision problems.
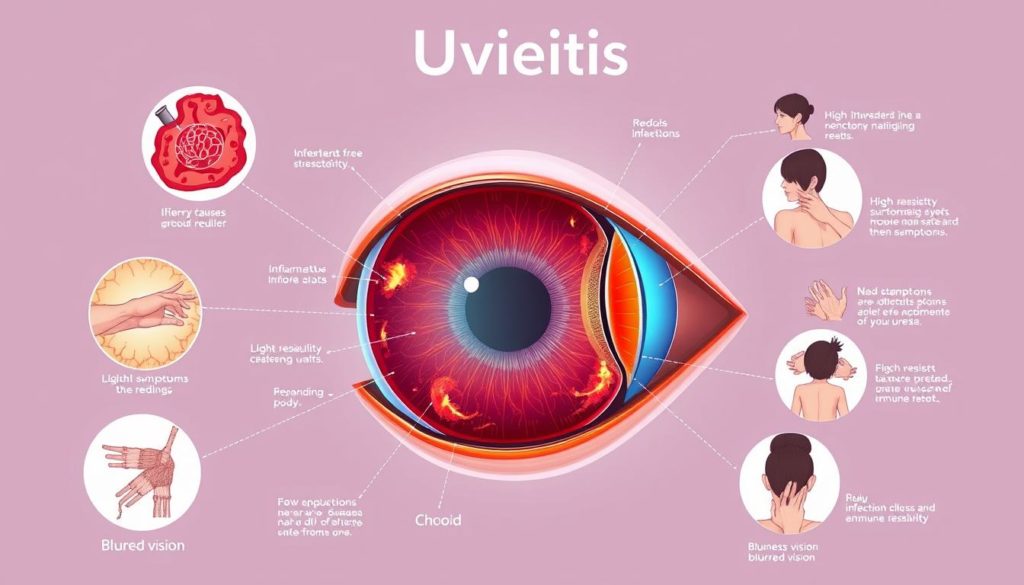
Let’s delve into what Uveitis truly means. It’s the inflammation of the uvea, the eye’s middle layer. This layer has the iris, ciliary body, and choroid. These parts are crucial. They supply blood to the retina, essential for sharp vision.
Uveitis Definition
Uveitis means inflammation anywhere in the uvea. Yet, it can also strike other eye areas like the lens, retina, optic nerve, and vitreous. To spot uveitis, look out for red eyes, pain, blur, and sensitivity to light.
Anatomy of the Eye: Where Uveitis Occurs
To grasp how uveitis affects vision, understanding the eye’s anatomy is vital. The primary spots hit by uveitis include:
- Iris: The eye’s colored part around the pupil, controlling light entry.
- Ciliary Body: This part creates eye fluid and helps the lens focus.
- Choroid: Situated between the retina and the sclera, it’s vital for delivering oxygen and nutrients to the retina.
When these areas get inflamed, vision effects can vary. They might be as mild as slight blurriness or as severe as losing sight. Catching and treating uveitis early is critical. It helps control its effects on your vision.
Recognizing the Symptoms of Uveitis
Knowing the early signs of uveitis is key for quick action. It helps avoid serious issues and get the right advice fast.
Common Uveitis Symptoms
Different symptoms may show up based on which part of the eye is affected. The usual uveitis symptoms are:
- Eye redness
- Pain in the eye
- Blurred vision
- Light sensitivity (photophobia)
- Floaters—small shapes or shadows seen drifting in the field of vision
These signs hint at inflammation in the eye. They call for a full uveitis diagnosis and a specific treatment plan.
When to Seek Medical Attention
If you spot any main signs of uveitis, especially if they come on fast or get worse quickly, see a doctor:
- Severe eye pain
- A noticeable decrease in vision
- Increasing eye redness
- Persistent discomfort despite over-the-counter treatment
Quick doctor visits are key. They greatly improve your chances for a good result in treating uveitis.
By noticing and acting on early signs of uveitis, you can really lower the risk of serious issues and protect your vision.
Different Uveitis Types and How They Affect the Eye
Understanding the various uveitis types is crucial. It helps us see how each type impacts vision and overall eye health.
Anterior uveitis, or iritis, affects the eye’s front part. It’s the most common form. Symptoms include redness, pain, and sensitivity to light. Intermediate uveitis impacts the vitreous, leading to blurry vision and floaters.
Posterior uveitis targets the eye’s back, focusing on the retina and choroid. This type can cause severe vision loss. Panuveitis affects all major eye parts and needs quick action due to its widespread effects.
| Type | Location Affected | Symptoms | Risk to vision |
|---|---|---|---|
| Anterior Uveitis | Front of the eye | Eye redness, pain, photophobia | Moderate |
| Intermediate Uveitis | Vitreous | Blurred vision, floaters | Low to moderate |
| Posterior Uveitis | Retina and choroid | Visual disturbances, possibly painless | High |
| Panuveitis | All parts of the eye | Combination of all symptoms | Very high |
Each type of uveitis has unique implications. They demand distinct approaches for management and treatment. This helps preserve eye health and vision.
Exploring the Causes of Uveitis
Looking into why uveitis happens means understanding many factors. This eye issue can be caused by things like infections and autoimmune disorders. It’s vital to know exactly what causes uveitis to treat it right.
Infections Leading to Uveitis
Infections are a big reason behind uveitis. Viruses like the herpes simplex and the varicella-zoster are often to blame. Also, bacterial infections like syphilis and diseases like tuberculosis can cause it. Even parasites, such as those from toxoplasmosis, are known to lead to uveitis.
Autoimmune Disorders and Uveitis
Autoimmune disorders play a big role in causing uveitis. Diseases like rheumatoid arthritis and lupus can make the immune system attack the eye. Knowing how these diseases link to uveitis is important for managing it.
Eye injuries and exposure to toxic chemicals are also factors. Sometimes, uveitis is a sign of cancer, known as masquerade syndrome because it looks like inflammation.
Diagnosing Uveitis: Tests and Procedures
Getting the right diagnosis for uveitis is key to treating it well. We’ll look at the various tests and steps doctors take to find and measure uveitis.
Eye Examination Details
A thorough eye exam is the first step in diagnosing uveitis. Eye specialists use different methods to check the inside of the eye. This is vital to see any signs of uveitis. Tests for seeing how sharp your vision is, and exams with a slit lamp to look at the front parts of the eye in detail, are common. They help spot inflammation or unusual cells and proteins in the eye, which suggest uveitis.
Imaging Techniques in Uveitis Diagnosis
Imaging is crucial in diagnosing uveitis. Tools like Optical Coherence Tomography (OCT) and Fluorescein Angiography are key. They check the structure of the retina and choroid to see how much the eye is inflamed.
| Imaging Technique | Purpose | Benefits |
|---|---|---|
| Optical Coherence Tomography (OCT) | To capture detailed cross-sectional images of the retina. | Allows high-resolution imaging of eye structures, helping in the identification of fluid accumulation and retinal layers’ inflammation. |
| Fluorescein Angiography | To visualize blood flow in the retina and choroid. | Effective in detecting vascular changes and leakage that are common in inflammatory conditions of the eye. |
These tests for uveitis are important not just for diagnosis. They also track how the disease changes over time and if treatments are working.
Uveitis Treatment Strategies and Medication
Managing uveitis well means combining medication with lifestyle changes. Treatments are custom-made for each person, focusing on their unique form of uveitis.
At the heart of uveitis treatment are corticosteroids to tackle inflammation. Sometimes, doctors also use other drugs like immunosuppressants or biological agents, depending on what’s causing the uveitis. Let’s look at some usual treatments:
- Topical steroids: Ideal for anterior uveitis.
- Injectable or oral steroids: Needed for inflammation in the middle or back of the eye.
- Immunosuppressive drugs: For those who don’t respond to steroids or need treatment for a long time.
- Biological agents: Useful for tough or complicated cases, targeting specific immune system parts.
Following your doctor’s treatment plan closely is key to control symptoms and avoid complications. Here’s a table with common meds and their uses:
| Medication Type | Description | Common Uses |
|---|---|---|
| Corticosteroids | Reduce immune activity and lower inflammation. | Comes in topical, injectable, or oral forms for different uveitis types. |
| Immunosuppressants | Curb the immune response that leads to inflammation. | For long-term control of chronic uveitis, avoiding steroids. |
| Biologic Drugs | Attack certain immune system elements causing inflammation. | For cases that resist treatment or specific diseases like Behçet’s. |
Medicine is vital in uveitis care, but so are lifestyle changes. This includes shielding your eyes from UV lights, reducing stress, and regular check-ins with your doctor. Together, these steps help make treatments work better and improve your life.
In conclusion, uveitis management always evolves. Patients need to work closely with their doctors. This helps find the best treatment plan for their individual needs.
Corticosteroids and Their Role in Uveitis Treatment
Corticosteroids in uveitis treatment are crucial because of their strong anti-inflammatory effects. They are key in handling sudden outbreaks and chronic types of this eye condition.
Side Effects and Usage Guidelines
Corticosteroids are very effective but must be used wisely. It’s essential to handle their usage to avoid side effects. Here are important tips for using corticosteroids in treating uveitis:
- Always follow dosage instructions from healthcare professionals closely.
- Monitor for common side effects such as increased eye pressure and cataract formation.
- Utilize corticosteroids in conjunction with other treatment forms to balance efficacy with safety.
| Corticosteroid | Formulation | Usage |
|---|---|---|
| Prednisone | Oral | Systemic treatment for severe uveitis |
| Triamcinolone | Injection | Administered directly into the eye for localized treatment |
| Dexamethasone | Implant | Slow-release formulation for extended control of inflammation |
For effective management of uveitis with corticosteroids, a careful treatment balance is needed. Following doctor’s orders and regular check-ups with an eye specialist are key for good results.
Non-Steroidal Approaches to Managing Uveitis
Doctors are finding new ways to treat Uveitis without always using steroids. They are turning to immunosuppressive therapy and biologic medicines. These options are getting popular because they target the problem better and usually have fewer negative effects.
Immunosuppressive Therapy
For severe Uveitis, or when steroids don’t work, immunosuppressive therapy is a game changer. It includes drugs like methotrexate, azathioprine, and cyclosporine. These drugs help calm the immune system. This way, it stops attacking the eye and reduces swelling without relying too much on steroids.
Biologic Medications and Future Treatments
Biologic medications, such as adalimumab and infliximab, have shown great results. They directly target parts of the immune system involved in Uveitis. This targeted approach can mean fewer side effects compared to other treatments. Ongoing studies will keep improving how we handle this condition.
These advancements are changing how we deal with Uveitis. They aim for longer-lasting solutions and less risk of the disease coming back. Every new discovery helps people with Uveitis live better lives. The goal is to lessen the symptoms and improve their overall well-being.
Lifestyle Adjustments for Living with Uveitis
Managing uveitis goes beyond just taking medicine. It includes changes in your lifestyle that can really help improve your life and symptoms. Knowing which changes to make is key for long-term control of uveitis.
Lifestyle adjustments are essential in a full uveitis management plan. Here are some top tips for those living with uveitis:
- Diet: Eat foods that fight inflammation like leafy greens, fatty fish, and whole grains. These help decrease inflammation in your body.
- Hydration: Drinking enough water is vital. It keeps your eyes healthy and helps manage symptoms.
- Exercise: Activities like walking or yoga can lower stress. Stress can make uveitis worse.
- Rest: Getting enough sleep helps your eye health. It helps manage symptoms of uveitis.
- Avoid Smoking: Smoking can increase inflammation and make uveitis symptoms worse.
These life changes not only help manage uveitis better but also boost overall health. Continuously learning about these adjustments is critical. It allows patients to actively manage their condition.
| Lifestyle Change | Benefits in Uveitis Management |
|---|---|
| Anti-inflammatory Diet | Reduces eye inflammation and symptoms |
| Regular Exercise | Decreases stress levels, which may trigger flare-ups |
| Adequate Rest | Supports eye health and recovery |
| Smoking Cessation | Lowers the risk of exacerbating inflammation |
Putting these habits into your daily routine can give you better control over uveitis. This leads to a more active and fulfilling life. Seeing your doctor regularly helps make sure these changes are working. It creates a plan that’s just right for your uveitis management.
Understanding Potential Uveitis Complications
Delving into uveitis, it’s vital to know about uveitis complications. These affect eye health and the uveitis prognosis. They shape life quality for those affected.
Complications That Can Arise
Improperly managed uveitis can cause several serious eye issues, such as:
- Cataracts – the lens becomes cloudy, leading to worse vision.
- Glaucoma – pressure increases in the eye, possibly harming the optic nerve.
- Macular edema – the central retina swells, impairing sharp vision.
- Retinal detachment – a serious situation where the retina disconnects from its place.
- Permanent vision loss – the most feared outcome, highlighting the importance of early care.
Long-term Outlook and Prognosis
Knowing the uveitis prognosis is crucial for patients. Prognosis factors include:
- Type of uveitis (anterior, intermediate, posterior, or panuveitis).
- How well treatment works, which differs in everyone.
- How quickly and consistently treatment begins after finding the disease.
- Overall health and other existing conditions.
Quick detection and right treatment help avoid lasting harm and improve prognosis. Thanks to medical advances and ongoing care, many with uveitis lead fulfilling lives.
Identifying and Treating Uveitis in Children
Diagnosing uveitis in children is tricky. They often can’t say what bothers them. Catching it early helps protect their vision against serious problems.
Signs and Symptoms: Uveitis in children might look like allergies or simple eye troubles at first. Watch out for redness, pain, not liking light, and blurry vision. If a child often complains about these, see a specialist right away.
- Medical Evaluation: A detailed check-up by a kid’s eye doctor is key to finding out what’s wrong. Checking for uveitis in children also means looking for other health issues, so knowing their full health story and examining them fully matters a lot.
- Treatment Approaches: How to treat uveitis in children depends on how bad it is and the cause. Reducing swelling with corticosteroids is usual, and sometimes doctors use medicine to calm the immune system too.
Keeping an eye on how the treatment is working is crucial. Regular check-ups help keep uveitis in children under control. This approach helps protect their sight and ensure they can enjoy life.
| Age Group | Symptoms Frequency | Treatment Adaptation |
|---|---|---|
| Toddlers (1-3 years) | Occasionally observed | Milder medications, regular monitoring |
| School-Age Children (4-12 years) | Commonly reported | Standard anti-inflammatory treatments |
| Teenagers (13-18 years) | Frequently observed | Combination of therapies possible |
In conclusion, proper care for uveitis in children can really make a difference. It can save a child’s vision and make their future brighter.
Can Uveitis Be Prevented?
While facing uveitis can be tough, knowing about uveitis prevention may help lower its risk. It is good to look into daily habits and health practices to protect our eyes.
Regular Eye Exams and Preventative Measures
Getting your eyes checked regularly is key for catching and uveitis prevention early. Finding and treating issues early on can greatly help in stopping uveitis or lessening its impact.
- Regular Eye Check-ups: Going to scheduled eye exams helps doctors find early signs of problems that could cause uveitis.
- Avoiding Eye Strain: Taking breaks from screens and using good lighting can reduce eye stress.
- Protective Eyewear: Wearing eye protection during certain activities can prevent irritants from harming the eyes.
These steps don’t fully ensure uveitis won’t happen, but they can greatly reduce its chances and effects. Always talk to your doctor if you experience eye discomfort or changes in vision to stay ahead in uveitis prevention.
| Preventative Measure | Benefit |
|---|---|
| Yearly Eye Examinations | Leads to early discovery of problems, allowing for prompt action. |
| Use of Sunglasses | Shields the eyes from harmful UV rays, preventing damage. |
| Maintaining a Healthy Diet | Provides essential nutrients like Vitamins A and C for eye health. |
The Importance of Early Intervention in Uveitis Cases
Understanding the importance of early action in Uveitis is key. Quick response helps manage symptoms well and prevents eye damage.
Benefits of Timely Diagnosis
Timely detection of Uveitis matters a lot. It lets doctors treat effectively early on. Early detection helps avoid worse vision problems or even vision loss.
Improving Treatment Outcomes
Early treatment of Uveitis means better chances for patients. It makes milder treatments more likely, reducing side effect risks. This also helps keep vision sharp and life quality high for those affected.
Early action in Uveitis does a lot for eye health and patient well-being. Here’s a detailed look at the advantages:
| Condition | With Early Intervention | Without Early Intervention |
|---|---|---|
| Treatment Efficacy | Highly effective, fewer complications | Reduced effectiveness, more complications |
| Visual Acuity | Likely preserved | Potential for significant loss |
| Quality of Life | Maintained at high level | Often significantly diminished |
The table shows clear benefits of early Uveitis care. Spotting symptoms early and getting help is key for those with Uveitis signs.
Advancements in Uveitis Research and Treatment
The study of uveitis is always moving forward. We’re finding better ways to understand and treat this complex eye problem. New therapies for uveitis are more effective and safer.
Researchers are zooming in on what causes uveitis. They’ve found markers that could lead to personal treatment plans. This is a big step towards helping patients get better, quicker.
Innovation is driving new treatment and surgery options. Biologics, for example, have changed the game for many patients. Let’s look at what’s new:
- Biologics reduce swelling without the side effects of corticosteroids.
- Implantable devices deliver drugs right where they’re needed. This makes treatment better and easier for patients.
- New surgical methods are safer and help patients recover faster.
| Advancement | Impact |
|---|---|
| Biologic Treatments | Target specific immune system pathways, cutting down inflammation with less harm. |
| Implantable Devices | They ensure steady, direct drug delivery, making treatments more successful and safer. |
| Refined Surgical Techniques | They’re less invasive and allow for quicker recovery, reducing risk. |
These advances in uveitis research and treatment are great news. They point towards care that’s focused on the patient, more effective, and kinder. With ongoing discoveries and tech, the future is bright for those dealing with uveitis.
Resources and Support for Uveitis Patients
Dealing with uveitis is tough, but you’re not alone. There’s a strong uveitis patient support network ready to help. This network is key for those fighting the condition. It offers moral support and useful tips. Becoming part of this community can really improve your life. It gives you the information you need to take charge of your health.
Support Groups and Education
Uveitis support groups are essential for patient wellness. They provide a space to share stories and advice. These groups also share important educational resources. They help patients understand how to live with and manage uveitis. You can find these groups online, in local meet-ups, or through healthcare providers. They offer coping methods, research updates, and new treatment options. This collective knowledge strengthens each member’s ability to cope.
Navigating Healthcare for Uveitis
Knowing how to manage uveitis care is key. Navigating uveitis healthcare is more than just doctor visits. It includes understanding insurance, finding specialists, and keeping up with new treatments. Better healthcare management leads to quick, precise diagnosis and access to the latest therapies. It ensures care is perfectly suited to each patient’s needs.
FAQ
What Is Uveitis?
Uveitis is inflammation of the eye’s middle layer, or uvea, which includes the iris, ciliary body, and choroid. It can cause symptoms like redness, pain, sensitivity to light, and blurry vision. If not treated, it can damage your vision and eye health.
What are common Uveitis symptoms?
If you have uveitis, you might notice your eye turns red and hurts. Your vision could get blurry, and you might be sensitive to light. How it affects you can vary based on the type of uveitis.
When should I seek medical attention for Uveitis?
You should get medical help if you have symptoms like eye redness, pain, blurry vision, or sensitivity to light. Especially if these symptoms are severe or come with a sudden loss of vision. Getting diagnosed and treated early is key to avoiding worse problems.
What are the different types of Uveitis?
Uveitis comes in different types based on where it occurs in your eye. Anterior uveitis is in the front part, intermediate affects the vitreous, posterior is at the back, and panuveitis impacts all layers of the uvea.
What causes Uveitis?
Uveitis can be caused by infections, like herpes or syphilis, or immune system disorders, such as rheumatoid arthritis or lupus. Eye injuries and certain diseases or cancers can also lead to uveitis.
How is Uveitis diagnosed?
To diagnose uveitis, doctors do a full eye exam and might run tests like blood work or imaging. They may also look at your eye’s fluids to find out what’s causing the inflammation.
What treatments are available for Uveitis?
Treating uveitis can involve medication, like steroids or drugs that suppress your immune system. Changes in your diet and stress management can help too. Sometimes, surgery might be needed. The treatment plan depends on your specific situation.
What are the possible side effects of corticosteroids used in Uveitis treatment?
Corticosteroids can cause side effects, such as higher eye pressure, cataracts, and a greater risk of infections. It’s important to use them exactly as your doctor instructs to avoid these issues.
Can Uveitis be effectively managed with immunosuppressive and biologic medications?
Yes. For those who can’t take steroids or need more help, immunosuppressive and biologic drugs can control Uveitis well.
How can lifestyle adjustments help in managing Uveitis?
A healthy lifestyle can support your eye health. This includes eating right, reducing stress, wearing sunglasses to block UV light, and not smoking.
What complications can arise from Uveitis?
Uveitis can lead to problems like cataracts, glaucoma, swelling of the retina, damage to the optic nerve, and loss of vision. Early and proper treatment is essential to prevent these.
What is the long-term outlook for someone with Uveitis?
With the right treatment, many people with uveitis can keep good vision. However, some might have ongoing inflammation or repeat episodes.
Can Uveitis Be Prevented?
While you can’t prevent all cases of uveitis, regular eye check-ups, managing overall health, and preventing infections can lower your risk.
Why is early intervention important in Uveitis cases?
Quick action is key because it stops inflammation, prevents damage, and saves your sight. Starting treatment early leads to a better outcome.
Are there advancements in Uveitis research and treatment?
Yes. Research into new drugs and treatments is making it easier to manage Uveitis, with fewer side effects and better results for patients.
Where can Uveitis patients find support and resources?
Support is available through groups, patient organizations, educational content, and healthcare professionals who specialize in eye care and uveitis.
What special considerations are there for treating Uveitis in children?
Treating kids involves carefully watching for side effects, protecting their growing vision, and working with specialists in children’s health.


